The World Health Organization ended mpox’s global emergency status on Sept. 5, citing sustained declines in key African hotspots, but warning the threat remains and standing recommendations continue to apply.
The decision followed advice from WHO’s Emergency Committee and was announced by Director-General Tedros Adhanom Ghebreyesus, who stressed that countries should “keep the urgency” even as the formal alert is lifted.
Globally, transmission has eased from its 2024 peak, yet the burden still sits largely in Africa. Based on WHO’s multi-country situation reports, there were 30,022 confirmed cases and 119 deaths worldwide from Jan. 1–June 30, 2025; within Africa alone, 28,152 confirmed cases and 133 deaths were logged across 24 countries in the year to July 20. In other words, the center of gravity remains on the continent even as surveillance elsewhere stays on guard.
Meanwhile, the virus’s evolutionary story keeps shaping the response. The present wave is driven by clade I—specifically clade Ib, with community transmission concentrated in Central and East Africa; nevertheless, travel-linked infections have been detected across Asia, Europe, the Middle East, Oceania, and the Americas, according to the U.S. Centers for Disease Control and Prevention (CDC).
China, for instance, reported a clade Ib cluster in early 2025, illustrating how importations can appear far from the African epicenter.
In the Philippines, case numbers are low but not negligible.
As of May 31, the Department of Health (DOH) said the country had recorded 911 mpox cases since 2024, even as May saw fewer cases than April, reinforcing the need for steady, not alarmist, vigilance. Late-2024 confirmations were clade II, and included local transmission in Metro Manila, according to DOH and Reuters reporting.
A HEALTH JOURNAL IS IMPORTANT SO YOU HAVE A RECORD WHEN YOU GET SICK.
A Shifting Epidemic Driven by Clade Ib
The outbreak profile in 2024–2025 differs from the 2022 clade II wave. WHO’s August 2024 declaration of a Public Health Emergency of International Concern (PHEIC) followed a sharp rise in the Democratic Republic of the Congo (DRC) and spread to countries with no prior mpox history, driven by clade Ib.
The agency warned then, and continues to emphasize now, that strengthened cross-border vigilance is essential.
By mid-2025, the CDC summarized the pattern bluntly: clade I outbreaks persisted across multiple Central and East African countries, with travel-associated cases documented in several world regions. On severity, CDC notes clade I has historically been more virulent than clade II, which helps explain why African datasets show higher fatality ratios than the global average during this emergency.
That gradient is reflected in the numbers. Based on WHO’s global update in May 2025, the overall case-fatality ratio was about 0.2% across 49 countries; by contrast, analyses of African outbreaks in 2024 reported higher ratios (around 1–3% in some summaries), consistent with clade and context.
A New England Journal of Medicine review of 2024 data, for example, underscored elevated severity in DRC’s clade I setting.
Regionally, Africa CDC still treats mpox as a continental emergency. Although weekly confirmed cases fell by roughly half between late spring and mid-summer 2025, fresh surges in Ghana, Liberia, Kenya, Zambia, and Tanzania, and new introductions in Malawi, Ethiopia, Senegal, Togo, The Gambia, and Mozambique, show how quickly declines can reverse if new chains of transmission take hold.
Vaccine Access Widened — But Supply, Equity, and Logistics Still Bite
Vaccine policy moved notably in late 2024. On Sept. 13, WHO prequalified Bavarian Nordic’s MVA-BN (marketed as Imvanex/Jynneos), the first mpox vaccine on the agency’s PQ list, opening procurement via UN channels; on Oct. 8, WHO extended that PQ indication to ages ≥12. Then on Nov. 19, WHO granted Emergency Use Listing (EUL) to Japan’s LC16m8, crucially authorized for use from age ≥1 year, important in settings where children bear a disproportionate burden.
Supply mechanisms also matured. UNICEF, working with Gavi, Africa CDC and WHO, launched an emergency tender on Aug. 31, 2024, to secure vaccine supply through 2025; within weeks, UNICEF reached an agreement to procure one million MVA-BN doses for African countries, with financing help from partners. Japan, for its part, committed 3.05 million LC16m8 doses (plus specialized needles) to the DRC.
However, agencies continue to flag cold-chain, financing, regulatory and pediatric-campaign logistics as practical bottlenecks—especially in the hardest-hit provinces.
The Philippines: Low Case Counts, Higher Stakes for Surveillance
If distance offers false comfort, preparedness is the antidote.
Here at home, Philippine mpox activity has stayed low. After a quiet first half of 2024, the Department of Health (DOH) confirmed new cases in August–September 2024, all clade II (the milder lineage linked to the 2022 global wave). These reports included the year’s first case with no travel history—evidence of local transmission in Metro Manila—followed by additional detections that brought active cases to 14 by September 9, 2024; no deaths were reported.
Why should that still concern us? This local picture still warrants vigilance because clade I, the lineage driving Africa’s crisis, has repeatedly seeded travel-linked cases across Asia, Europe, the Middle East, Oceania, and the Americas, based on the U.S. CDC’s global situation update (as of Aug. 6, 2025).
To reinforce preparedness, DOH’s Department Memorandum 2024-0306 (Aug. 26, 2024) consolidated case definitions, infection-prevention guidance and reporting templates nationwide, frameworks that regional offices and schools have echoed since. Meanwhile, the Research Institute for Tropical Medicine (RITM) updated specimen collection and shipping protocols in mid-August and early September 2024, emphasizing lesion-swab prioritization and a 2–8 °C cold chain to speed accurate PCR results. At the borders, the Bureau of Quarantine issued interim mpox guidelines on Aug. 27–28, 2024 to align screening, isolation and referral.
Philippine institutions also stress the 21-day window for contact follow-up. WHO’s surveillance guidance specifies daily monitoring of close contacts for 21 days from last exposure, a standard echoed in local briefings. And in March 2025, the Philippines led the Western Pacific by convening the region’s first mpox intra-action review (IAR) to pressure-test surveillance, border measures and risk communication in real time.
Why Clade I Matters Clinically — and What to Tell Patients
Clade designations aren’t semantics. According to CDC, clade I has historically produced more severe disease than clade II; in the 2024–2025 African outbreaks, children have shouldered a notable share of severe outcomes, shaped by household spread and health-system constraints.
Nevertheless, the prevention message to the public remains the same across clades: limit close skin-to-skin contact when someone has a suspicious rash, seek prompt testing, and isolate until all lesions have healed with fresh skin.
Key Takeaways for Frontline Facilities in the Philippines:
- First, keep clade I on the differential when a rash-illness patient reports recent travel to affected African countries, or close contact with travelers, given ongoing exportations described by CDC.
- Second, follow RITM’s updated packaging and cold-chain instructions (2–8 °C) for lesion swabs to avoid delays.
- Third, trigger case investigations and ensure 21-day contact monitoring per WHO guidance, using DOH’s forms to keep investigations consistent and complete.
Communications Challenges: Stigma, Behavior, and Trust
The 2022 clade II wave showed how stigma can derail response, especially when transmission amplifies in specific sexual networks. WHO has repeatedly cautioned against blame-focused messaging, urging risk-based, inclusive communication.
The European Centre for Disease Prevention and Control’s 2025 advice aligns with this approach. In clade I-affected areas, where women and children comprise sizable shares in some datasets, household-focused prevention and trusted, practical messaging are essential.
For local governments, that translates into clear, plain-language advisories on rash-illness recognition and when to seek care; privacy-respecting contact tracing and support for isolation; and partnerships with schools, barangays and civil-society groups to counter misinformation.
WHO’s Western Pacific office points to the Philippines’ March 2025 IAR as an example of proactive risk communication and multi-sector coordination.
Are Vaccines Coming to the Philippines?
Policy doors are open, but supply is prioritized to where need is greatest. DOH said in September 2024 there was no FDA-approved mpox vaccine in the Philippines, and as of June 2025 the Philippine Society for Microbiology and Infectious Diseases noted that antivirals, immunoglobulin, and vaccines were not available locally.
Given global allocation choices and the country’s low, clade II-dominant caseload, targeted access, such as post-exposure prophylaxis for high-risk contacts of imported cases, remains the most plausible near-term scenario, consistent with WHO and CDC guidance on PEP timing.
What Travelers and Enterprises Should Know
Travelers: There are no general travel bans tied to mpox. But risk is not zero.
If your itinerary includes Central or Eastern Africa, or you have close contact with travelers from affected areas, treat any unexplained rash, fever, or swollen lymph nodes as a cue for immediate medical consultation and testing; avoid close skin-to-skin contact and isolate pending results.
Employers and schools: In late 2024, DOH circulated workplace and home-isolation guidance to help organizations prevent and respond to suspected cases, building on the updated national memorandum.
Review sick-leave policies, confidential reporting channels, and cleaning protocols for high-touch surfaces; train staff to recognize symptoms and refer promptly.
The Surveillance Test We Can’t Afford to Fail
COVID-era upgrades-built muscle memory that mpox continues to test. The backbone now is quick detection (and the logistics that make it possible), standardized case investigations, reliable 21-day contact monitoring, and event-based surveillance at ports—kept sharp with drills and refreshers.
Just as importantly, transparent and non-alarmist communication sustains public trust.
The Philippines’ first-in-the-region mpox IAR in March 2025 shows how to keep those muscles conditioned.
- Rapid detection matters. WHO’s surveillance guidance is explicit: “As soon as a suspected case is identified, contact identification and forward contact tracing should be initiated,” and contacts should be monitored daily for 21 days, a standard designed to keep single importations from becoming clusters.
On the lab side, RITM’s updated specimen guidelines (Aug 16 and Sept 2, 2024) require that mpox specimens arrive cold at 2–8 °C and detail packaging and shipping steps—operational levers that speed confirmation.
- Standardized case investigation prevents blind spots. The DOH Department Memorandum 2024-0306 (Aug 26, 2024) consolidates national case definitions, IPC and reporting tools for mpox; paired with WHO surveillance guidance, it anchors 21-day contact monitoring and uniform case investigation to avoid blind spots.
CDC clinical/IPC pages echo the 21-day monitoring window for exposed persons in healthcare and community settings.
- Event-based surveillance at ports. The Bureau of Quarantine (BOQ) issued Interim Guidelines for the Implementation of Mpox Surveillance, Screening, Management and Infection Control on Aug 27–28, 2024, spelling out screening, isolation and referral pathways at points of entry—keeping the “watchtower” role of ports active.
- Transparent, non-alarmist communication sustains trust. WHO’s stigma and discrimination advisory (Nov 18, 2024) warns that blaming groups undermines case-finding and care-seeking, and recommends inclusive, risk-based language. 2025 public-health advice similarly centers on practical, behavior-focused guidance (isolation until lesions heal, household precautions, regular follow-up), not labels. WHO Western Pacific also reports the Philippines conducted the Region’s first mpox intra-action review (Mar 12–13, 2025) to improve surveillance, border measures and risk communication, a concrete step to keep trust high.
Bottom Line for the Philippines
The clade Ib emergency has eased enough for WHO to lift the global alert, yet Africa CDC still treats mpox as a continental emergency and CDC continues to log travel-associated clade I cases outside Africa.
The Philippines’ late-2024 detections were clade II and limited, but they included local transmission—proof that vigilance is non-negotiable. Vaccines are finally on the global table (MVA-BN PQ; LC16m8 EUL), with early supply triaged to African epicenters; domestically, execution, more than stockpiles, will determine outcomes: ship cold, test fast, monitor contacts for 21 days, and communicate without stigma.
That way, when the next alert comes, the response arrives in hours, not headlines.
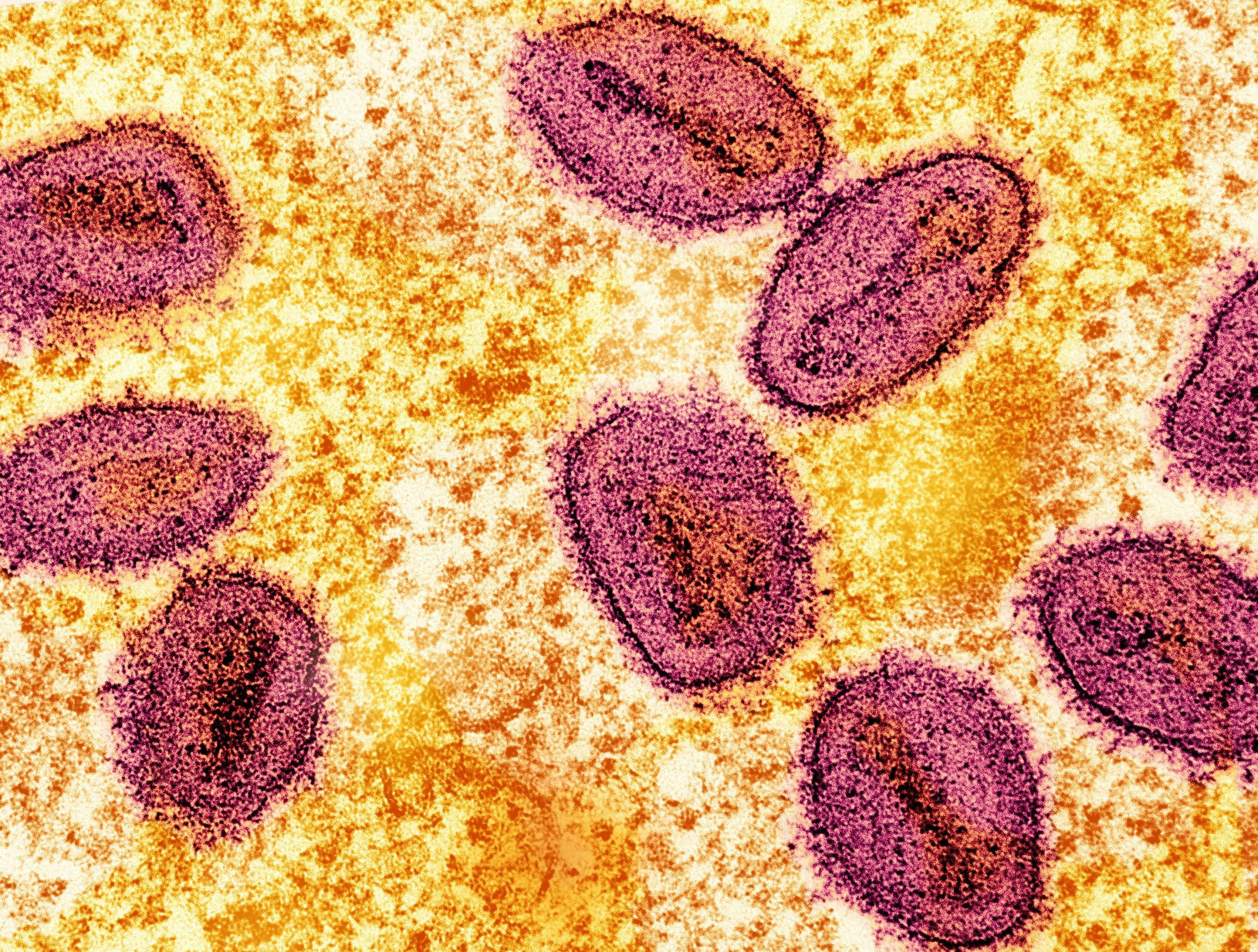
Photo by National Institute of Allergy and Infectious Diseases on Unsplash
DISCLAIMER
This article provides general information and does not constitute medical advice. Consult your healthcare provider for personalized recommendations. If symptoms persist, consult your doctor.